In its present form the National Health Scheme will continue
to reward state incompetence while assuming all private doctors are out
to cheat the system
 By Dr Marinos Soteriou
By Dr Marinos Soteriou
The entire philosophy of the National Health Scheme (Gesy) is based on a fixed budget divided by a finite number of medical procedures, resulting in a unit price to be paid per procedure. It is a mechanism to avoid abuse of the system by doctors tempted to perform unnecessary procedures to increase their gains.
Unfortunately, as a consequence, the system creates an unfair
situation where upright doctors could suffer financial consequences from
renegade physicians who unnecessarily try toincrease their revenues by
performing an increased number of procedures, thus reducing the unit
prices. The Health Insurance Organisation (HIO), which will manage Gesy,
will define the unit prices in retrospect, namely at the end of the
month and often long after the medical procedures have been completed.
This ensures the medical world does not refuse to provide medical care
because reimbursement is low. In reality it is a way of cheating doctors
and hospitals into performing procedures without knowing their true
reimbursement. I find this completely unfair and unacceptable.
The problem of course is the variation of the unit price, which may be dangerously low, or even below cost. It has to be understood that even a small variation in the unit price – say five to ten per cent – could result in below cost reimbursement and thus in major financial losses. Obviously the public hospitals will be shielded from such outcomes through government subsidies. In contrast, the private sector will receive no such financial assistance.
The HIO is claiming that armed with the Mercer study – which provided the blueprint for Gesy – and specially designed software that cost tens of millions of euros, it will be able to introduce and monitor protocols, guidelines, results, quality, payments and budgets. In addition we are told that the Mercer study is very detailed and precise, and that it made predictions for all variables. In that case it is reasonable to conclude that the HIO should be in position to introduce a stable, easily monitored unit price that does not exceed the budget. But the HIO is not willing to accept this responsibility and just chooses to penalise the doctors as a group in case of increased demand. In reality doctors who perform their duties with care and caution will be penalised for the abuses of renegade colleagues or hospitals which abuse the system.
In principle all doctors in Cyprus, both the private and public sector, will become employees of Gesy. Yet private physicians will not be granted any benefits associated with such employment, such as working hours, maternity or sick live. If physicians fall sick or shortly after delivery of a child, they will simply have no income. This is an unacceptable development in a “European country “.
Gesy is heavily weighted in favour of the state hospitals, which will continue to be inefficient and uncompetitive because they will be subsidised by the state for between three to five years, or even longer if needed, after Gesy is introduced.
Public hospitals may be paid the same rates as private hospitals, but if there is a big financial hole at the end of the year the state will cover it with additional taxpayer money. What incentive would a state hospital have to keep costs down and improve quality? It is the same anachronistic system that always favours state organisations and state employees.
The unfair competition will continue because the public employees at state hospitals will receive their pay rises every year, pushing up the costs in private hospitals as well, because we will have to follow suit to keep our staff. But we will not receive a state subsidy at the end of the year to cover any deficits caused as result.
If a private hospital runs an accident and emergency department operating 24/7, there will be a copayment charge fee of €10 per visit for the user. Once Gesy is introduced, there will be no charge for visiting the state owned outpatient clinics that will operate until midnight which puts us as at a disadvantage. So in reality up to midnight people are incentivised to use the state owned departments.
There is even a special law for private hospitals that dictates minimum safety requirements. Take an intensive care unit as an example. Private hospitals are obliged to have one bed every 12 square metres to reduce the risk for infections. The state hospital usually have multiple patients in the same area. All these things, plus many others add to costs. The state sets minimum standards for the private sector in order to safeguard patient safety, but the state-run hospitals are not required to meet these standards.
By default this results in major quality differences in the healthcare provided by the two sectors and inevitably results in “double standards“.
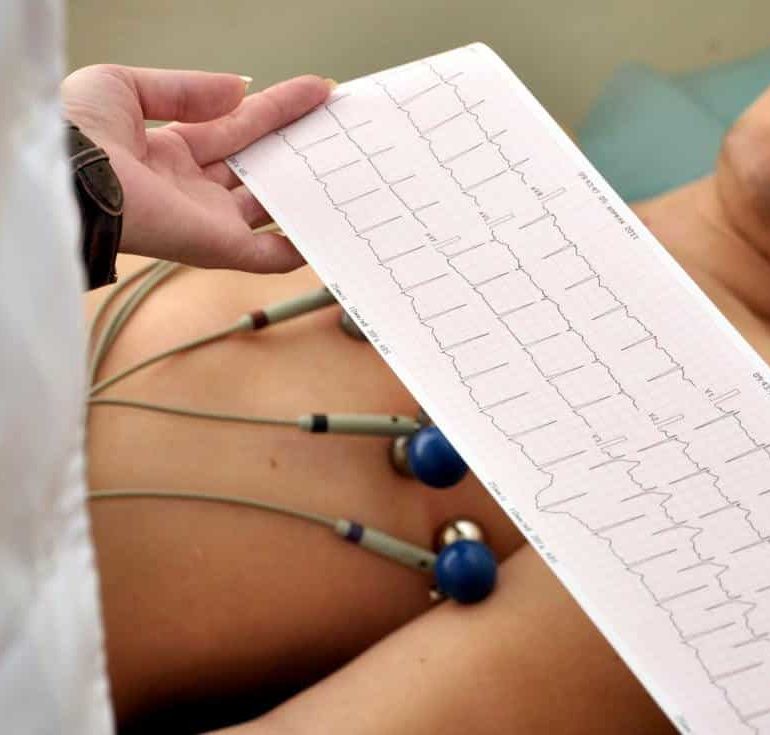
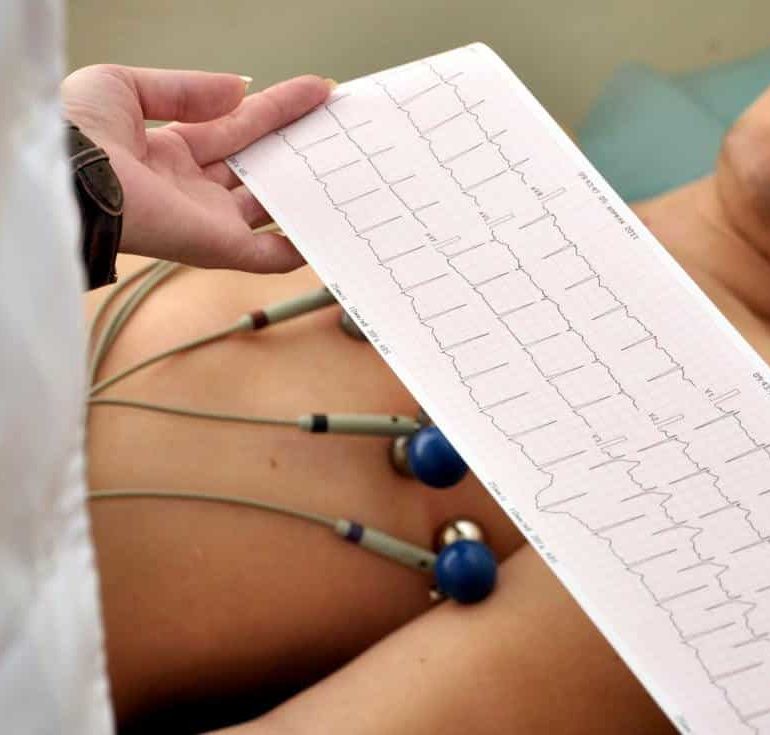
For example Gesy will pay €7.50 for an electrocardiogram. A manicurist receives €20 to do someone’s nails. I believe that it is unreasonable for society to accept that a doctor is paid less than a manicurist. We have to keep in mind the responsibility associated with reading the electrocardiogram and the risk to the patient and most certainly the financial consequences of malpractice costs if the doctor misses something. There was a relevant case recently in which a private hospital and a doctor were ordered by court to pay €750,000 in damages.
It is of paramount importance to understand that if the doctors are not properly rewarded, very soon the system will not be in position to recruit well trained, competent and experienced physicians, based on the dictum “if you pay peanuts you get monkeys “. The system will deter good physicians and attract incompetent ones. Similar developments have been recently observed in Greece, Germany and elsewhere.
There are other issues as well. For instance, the case of new therapies that are very expensive. For metastatic lung cancer there are two different therapies: chemotherapy that has very low chance for survival beyond one year and immunomodulation therapy that has kept a significant percentage of patients disease free and alive up to eight years so far. Immunomodulation is much more expensive (€100,000). If Gesy cannot cover the cost of immunomodulation, the doctors or the hospitals affiliated with Gesy are not allowed to accept co-payment from the patient to cover the extra cost. The HIO prohibits co-payment and makes the doctors liable.
We have invested in equipment that carries out mammography examinations for detection of breast cancer. At the rates Gesy will reimburse per examination, it will take 30 years to make our money back. How can we invest in the latest technology under such circumstances?
HIO is reimbursing all the doctors and all the hospitals at the same unit price. Sophisticated tertiary care centres with complex and expensive infrastructure and quality certification will receive the same reimbursement as smaller units that do not have the complexity and the expenses of the larger units. Quality care and patient safety for the patients and become a disincentive.
When we challenged the HIO about its practices, it cites the Mercer Study, but refuses to release the full study to be reviewed. There is only a summary on the health ministry website. The assumptions and other details of the study are still treated as a state secret. It is highly likely that the study contains a lot of information, principles and assumptions that do not correlate with what is about to be implemented through Gesy.
I am very concerned that the preparation for Gesy is very superficial, incomplete, unfair and biased. There has been an organised media campaign to blame and stigmatise doctors and push them to accept Gesy . Yet, it is now more than obvious that Gesy is poorly planned, poorly funded and will be badly executed with far reaching financial, accessibility and quality implications.
The authorities are in full denial of the imminent disaster and are not willing to address the situation. Only if the majority of physicians and private hospitals refuse to join Gesy will the authorities be forced into action
Dr Marinos Soteriou is a cardiothoracic surgeon and founder of the American Medical Center
The entire philosophy of the National Health Scheme (Gesy) is based on a fixed budget divided by a finite number of medical procedures, resulting in a unit price to be paid per procedure. It is a mechanism to avoid abuse of the system by doctors tempted to perform unnecessary procedures to increase their gains.
The problem of course is the variation of the unit price, which may be dangerously low, or even below cost. It has to be understood that even a small variation in the unit price – say five to ten per cent – could result in below cost reimbursement and thus in major financial losses. Obviously the public hospitals will be shielded from such outcomes through government subsidies. In contrast, the private sector will receive no such financial assistance.
The HIO is claiming that armed with the Mercer study – which provided the blueprint for Gesy – and specially designed software that cost tens of millions of euros, it will be able to introduce and monitor protocols, guidelines, results, quality, payments and budgets. In addition we are told that the Mercer study is very detailed and precise, and that it made predictions for all variables. In that case it is reasonable to conclude that the HIO should be in position to introduce a stable, easily monitored unit price that does not exceed the budget. But the HIO is not willing to accept this responsibility and just chooses to penalise the doctors as a group in case of increased demand. In reality doctors who perform their duties with care and caution will be penalised for the abuses of renegade colleagues or hospitals which abuse the system.
In principle all doctors in Cyprus, both the private and public sector, will become employees of Gesy. Yet private physicians will not be granted any benefits associated with such employment, such as working hours, maternity or sick live. If physicians fall sick or shortly after delivery of a child, they will simply have no income. This is an unacceptable development in a “European country “.
Gesy is heavily weighted in favour of the state hospitals, which will continue to be inefficient and uncompetitive because they will be subsidised by the state for between three to five years, or even longer if needed, after Gesy is introduced.
Public hospitals may be paid the same rates as private hospitals, but if there is a big financial hole at the end of the year the state will cover it with additional taxpayer money. What incentive would a state hospital have to keep costs down and improve quality? It is the same anachronistic system that always favours state organisations and state employees.
The unfair competition will continue because the public employees at state hospitals will receive their pay rises every year, pushing up the costs in private hospitals as well, because we will have to follow suit to keep our staff. But we will not receive a state subsidy at the end of the year to cover any deficits caused as result.
If a private hospital runs an accident and emergency department operating 24/7, there will be a copayment charge fee of €10 per visit for the user. Once Gesy is introduced, there will be no charge for visiting the state owned outpatient clinics that will operate until midnight which puts us as at a disadvantage. So in reality up to midnight people are incentivised to use the state owned departments.
There is even a special law for private hospitals that dictates minimum safety requirements. Take an intensive care unit as an example. Private hospitals are obliged to have one bed every 12 square metres to reduce the risk for infections. The state hospital usually have multiple patients in the same area. All these things, plus many others add to costs. The state sets minimum standards for the private sector in order to safeguard patient safety, but the state-run hospitals are not required to meet these standards.
By default this results in major quality differences in the healthcare provided by the two sectors and inevitably results in “double standards“.
For example Gesy will pay €7.50 for an electrocardiogram. A manicurist receives €20 to do someone’s nails. I believe that it is unreasonable for society to accept that a doctor is paid less than a manicurist. We have to keep in mind the responsibility associated with reading the electrocardiogram and the risk to the patient and most certainly the financial consequences of malpractice costs if the doctor misses something. There was a relevant case recently in which a private hospital and a doctor were ordered by court to pay €750,000 in damages.
It is of paramount importance to understand that if the doctors are not properly rewarded, very soon the system will not be in position to recruit well trained, competent and experienced physicians, based on the dictum “if you pay peanuts you get monkeys “. The system will deter good physicians and attract incompetent ones. Similar developments have been recently observed in Greece, Germany and elsewhere.
There are other issues as well. For instance, the case of new therapies that are very expensive. For metastatic lung cancer there are two different therapies: chemotherapy that has very low chance for survival beyond one year and immunomodulation therapy that has kept a significant percentage of patients disease free and alive up to eight years so far. Immunomodulation is much more expensive (€100,000). If Gesy cannot cover the cost of immunomodulation, the doctors or the hospitals affiliated with Gesy are not allowed to accept co-payment from the patient to cover the extra cost. The HIO prohibits co-payment and makes the doctors liable.
We have invested in equipment that carries out mammography examinations for detection of breast cancer. At the rates Gesy will reimburse per examination, it will take 30 years to make our money back. How can we invest in the latest technology under such circumstances?
HIO is reimbursing all the doctors and all the hospitals at the same unit price. Sophisticated tertiary care centres with complex and expensive infrastructure and quality certification will receive the same reimbursement as smaller units that do not have the complexity and the expenses of the larger units. Quality care and patient safety for the patients and become a disincentive.
When we challenged the HIO about its practices, it cites the Mercer Study, but refuses to release the full study to be reviewed. There is only a summary on the health ministry website. The assumptions and other details of the study are still treated as a state secret. It is highly likely that the study contains a lot of information, principles and assumptions that do not correlate with what is about to be implemented through Gesy.
I am very concerned that the preparation for Gesy is very superficial, incomplete, unfair and biased. There has been an organised media campaign to blame and stigmatise doctors and push them to accept Gesy . Yet, it is now more than obvious that Gesy is poorly planned, poorly funded and will be badly executed with far reaching financial, accessibility and quality implications.
The authorities are in full denial of the imminent disaster and are not willing to address the situation. Only if the majority of physicians and private hospitals refuse to join Gesy will the authorities be forced into action
Dr Marinos Soteriou is a cardiothoracic surgeon and founder of the American Medical Center
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου